Autoimmune diseases now impact more than 2 million Canadians. And with most autoimmune diseases on the rise in Canada and around the globe, getting the right help can be challenging, particularly if you’ve just lost your doctor or are without an assigned specialist to help.
Your Body and Immunity
Your body’s defense against illness and disease is the immune system. It works hard to protect your cells and keep out infection. Think of it as the army of organs, tissues, and cells that work together to keep you healthy and help you heal.
Now, imagine your body turning against itself, attacking its own tissues and organs. Your immune system goes rogue, erratic, and does not follow the rules. This invisible battle inside your body is known as autoimmune disease, and its efforts to add more Canadians to its numbers shows no signs of easing up. And yet, we still don’t know exactly why this happens.
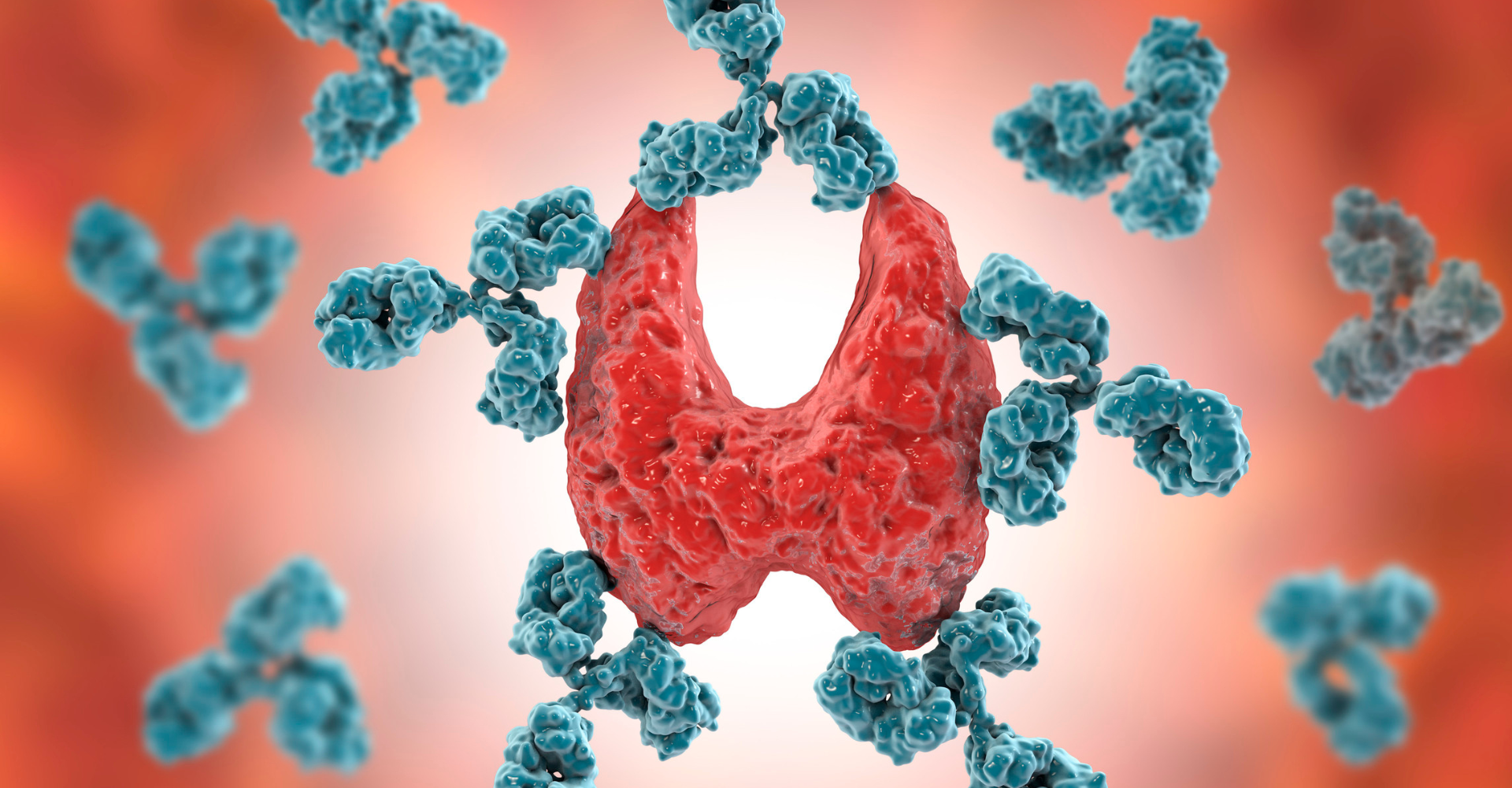
With a normal immune system, antigens are present on cells and viruses as markers to tell your immune system that there is a threat. Antibodies are then created to attack these cells and rid the system of these foreign threats.
With an abnormal immune system, autoantigens are created on otherwise normal cells. The results in the creation of the autoantibodies which attach these normal cells. This scenario is what is called an autoimmune disorder.
There are over 100 known autoimmune diseases. They can affect any organ or tissue.
Common Autoimmune Diseases
- Type 1 Diabetes: occurs when the pancreas does not make the insulin needed to help get glucose into the cells to give them energy. Without insulin, glucose stays in our blood, and when this happens, you can develop serious problems with your heart, eyes, kidneys, nerves, teeth, and gums.
- Rheumatoid arthritis: the immune system attacks the joints, causing inflammation, pain, and stiffness that can result in physical disabilities.
- Multiple Sclerosis: affects the brain and spinal cord. The messages between brain and body are slowed or blocked due to damage to the protective coating that surrounds the central nervous system.
- Lupus: can affect almost every organ in your body, causing inflammation and pain.
- Inflammatory Bowel Disease (Crohn’s/Colitis): affects the bowels, causing inflammation of the lining of the gastrointestinal tract. In Crohn’s, any part of the GI tract can be affected. With Colitis, the large intestine and rectum are affected.
Symptoms can come and go in many autoimmune diseases. They can be mild at times or severe. Flare-ups are the sudden onset of symptoms. When these happen, it is important to understand the triggers surrounding them. When you know the triggers, you can be proactive and see your doctor for appropriate treatment. Remission is the “normal” state or the time when you are not experiencing any symptoms.
Who is at Risk?
Autoimmune disease can affect anyone, and according to the Cleveland Clinic, the following factors increase your risk:
- Sex – females tend to present more with autoimmune disease
- Genetics – if you have family members diagnosed with an autoimmune disease
- Obesity – correlates to the inflammation that threatens the immune system
- Certain Medications – if you are taking blood pressure medication, antibiotics or statins (cholesterol medication)
- Viral/Bacterial infections – can trigger your immune system to self-attack
- Environment – smoking, air pollution, and UV radiation can impact the immune system
- Have one autoimmune disease already
Diagnosing an Autoimmune Disorder
Establishing a diagnosis for an autoimmune disease can be difficult. Blood tests are conducted to determine the amount of antibodies present. If you have these marker antibodies, you may have an autoimmune disease. The symptoms often mimic a variety of conditions, so pinpointing exactly what is going on can be a long-drawn-out process.
Treatment Options
Autoimmune disease involves long-term treatment specific to an individual’s environment, genetics, and immune system. Many symptoms can be managed using painkillers, anti-inflammatories, insulin injections, plasma exchanges, and corticosteroids.
Immunosuppressants and biologics slow or stop inflammation. Biologics are made from biological materials and can target specific parts of the immune system, whereas chemical-derived immunosuppressants suppress the whole immune system.
The cost of biologic medication can average anywhere from $10,000 to $20,000 annually. Biosimilar biologic drugs offer a less costly alternative. These drugs are similar to the original biologic drug and are available once the patent on the biologic has expired.
Monoclonal antibodies are laboratory-made and work like our natural antibodies to help target one specific antigen (threat). These antibodies are administered intravenously to help treat the body’s response to the autoimmune disease.
In Canada, out-of-pocket costs for autoimmune treatments can vary widely depending on the specific autoimmune disease, the type of treatment, and whether the treatment is covered under provincial medicare or through private insurance. In most cases, there is assistance available for Canadians unable to meet the financial obligation on their own.
Exciting and Emerging Research
There is some very exciting innovation going on in the field of autoimmune research. Recently, Penn State College of Medicine developed an algorithm using genetics and AI to identify any genetic patterns or risk factors that could be missed using traditional detection methods. By improving the accuracy of predictions, this AI algorithm can assist in earlier diagnosis of autoimmune disease and help create individualized treatment plans, which could lead to far better patient outcomes.
Another approach being studied is CAR T cell therapy, which is a treatment used for certain cancers. This therapy involves using the patient’s own immune cells (T cells) and altering them in a lab. The cells are then reinfused into the patient to target and attack the harmful cells in the body. Scientists are using this research to develop treatments for autoimmune conditions whereby they can modify the cells by eliminating or decreasing the likelihood of the body attacking its own cells.
An exciting initiative out of the University of Chicago, the “inverse vaccine” is in safety trials to treat Type 1 Diabetes, Rheumatoid Arthritis, Multiple Sclerosis, and Crohn’s. Normal vaccines trigger the immune system to fight off disease. An inverse vaccine works at ignoring the identified cells that are normally mistaken as harmful in autoimmune diseases. This treatment targets the specific cell versus suppressing the immune system, as in immunosuppressant therapies.
As we continue to see an increase in autoimmune diseases and the effects they have on individuals, families, and healthcare, more research and resources are required to better understand diagnostic, therapeutic, and preventative measures.
Autoimmune diseases are complex and, without a definitive cure, they can make day-to-day life challenging for those affected. Advances in research and technology offer hope for earlier and more accurate diagnoses, as well as new treatments, management, and possible cures that will improve quality of life.
Most of the common autoimmune diseases have corresponding research foundations and associations that share resources for understanding and treatment, along with lists of clinical trials going on in the specific area.
In addition to getting the proper medical attention where available, you’ll want to be sure that you’re doing your part to stay on top of the body of knowledge that exists and the experiences of others who have had more experience in the management and control of their condition.
The information provided on TheHealthInsider.ca is for educational purposes only and does not substitute for professional medical advice. TheHealthInsider.ca advises consulting a medical professional or healthcare provider when seeking medical advice, diagnoses, or treatment. To read about our editorial review process click here.