Birth control has been used for much longer than we can imagine. With its origins in 384 B.C. where the Greek philosopher Aristotle proposed the use of cedar oil as a spermicide, it can be said without a doubt that the scientific community has come a long way in the world of birth control.
One common birth control technique that gained popularity in 1960 was the birth control pill.
Despite this growing popularity, Canada did not permit marketing or prescribing the pill for birth control purposes until nine years after its approval due to birth control being illegal in Canada until July 1st , 1969.
Ever since legalization, rapid progression in scientific knowledge and technological advancements have paved the way for a variety of novel birth control techniques.
For example: the introduction of IUDs in 1988, plan B in 1999, and, more recently, hormone-free options.
The diverse spectrum of birth control options can make it difficult to know which one is best for you.
As with any decision, the first step involves learning about the various options. Join The Health Insider team as we explore innovations in birth control, empowering you to make an educated and confident decision.
Hormonal Methods for Consideration
The majority of hormonal contraception methods tweak the levels of estrogen and progestin in our bodies.
These two hormones are involved in stimulating ovulation and fertilization. By increasing levels of estrogen in the body, other crucial hormones which aid in the maturation of the egg, such as follicle-stimulating hormones (FSH), are inhibited.
Check out the following options for more information:
- Long acting vaginal ring
The vaginal ring can be inserted into the vagina in the privacy of a woman’s own home. With effects lasting for up to a month, this ring releases estrogen and progestin which prevents the release of an egg during ovulation. The vaginal ring has an efficacy of 99 per cent with a 0.3 per cent pregnancy rate as proven by a 2012 research study.
Common side effects include:
- Spotting and bleeding (only in the first few months)
- Increased vaginal discharge
- Headaches and nausea
- Breast tenderness
- Mood changes
The vaginal ring has also been associated with risks such as a slight increase in risk of developing breast cancer and blood clots. However, these are rare and can be resolved by halting the use of the ring.
Check out the table at the end of this section to see availability in Canada.
- Hormone patch
The hormone patch is a commonly used hormonal technique. This patch must be changed every week for three weeks and taken off on the fourth week.
Apply the patch anywhere on the skin. Avoid placement on irritated skin, the breasts, and skin which can be rubbed by tight clothing. Like the vaginal ring, the hormone patch also showed 99 per cent efficacy in clinical trials when used correctly.
Common side effects include:
- Skin irritation and soreness
- Nausea
- Spotting and bleeding
- Breast tenderness
- Mood changes
Many of these side effects, such as spotting and bleeding, resolve naturally within two to three months of use.
Common risks include increased cancer risk and blood clots, however these are extremely rare.
The following individuals should consider consulting their healthcare provider before using the hormonal patch:
- Smokers
- Individuals with regular migraines
- History of blood clotting
- Progestin pills
As the name suggests, this pill works by releasing the hormone progestin in the body which in turn thickens the mucus in the cervix to block sperm. This pill must be taken everyday for it to work with an efficacy of 99 per cent. This can drop to 91 per cent if not consumed perfectly. To ensure perfect use, consider the following suggestions:
- 3-hour progestin-only pill
- A pill must be taken within 3 hours of the same time each day
- 12-hour progestin-only pill
- A pill must be taken within 12 hours of the same time each day
Common side effects include:
- Irregular periods
- Spotting
- Acne, nausea, and headaches
- Cysts (usually harmless)
The progestin only pill has shown to increase the incidence of ovarian cysts which usually resolve themselves.
If pain persists over two months of use, consult your healthcare provider. While there is little known about the pill’s association with cancer, it is projected that it will be low, as seen with various other hormonal options.
- Male contraceptive pills
This pill must be taken daily for a month to effectively reduce sperm production. Mild side effects may be noted such as acne, headaches, and a reduced sex drive. However, these tend to resolve themselves over time.
Common risks revolve around blood clotting and reduction in sperm quality, however occurrence of these in clinical trials were considered rare.
Overall, the male contraceptive pill is considered safe, with an efficacy of 99 per cent and failure rate of 1.4 per cent.
- Testosterone transdermal gel
This gel works to inhibit sperm production and maintain sexual drive and function. The gel should be applied to the shoulders and upper arms for effective results. More notably, it is reversible; sperm levels return to normal about four months after use is halted.
The gel has gained popularity among individuals participating in its trials. While it remains in the research phase, and has a long way to go before it can come to the market, results thus far give us a great reason to be optimistic for this novel technique.
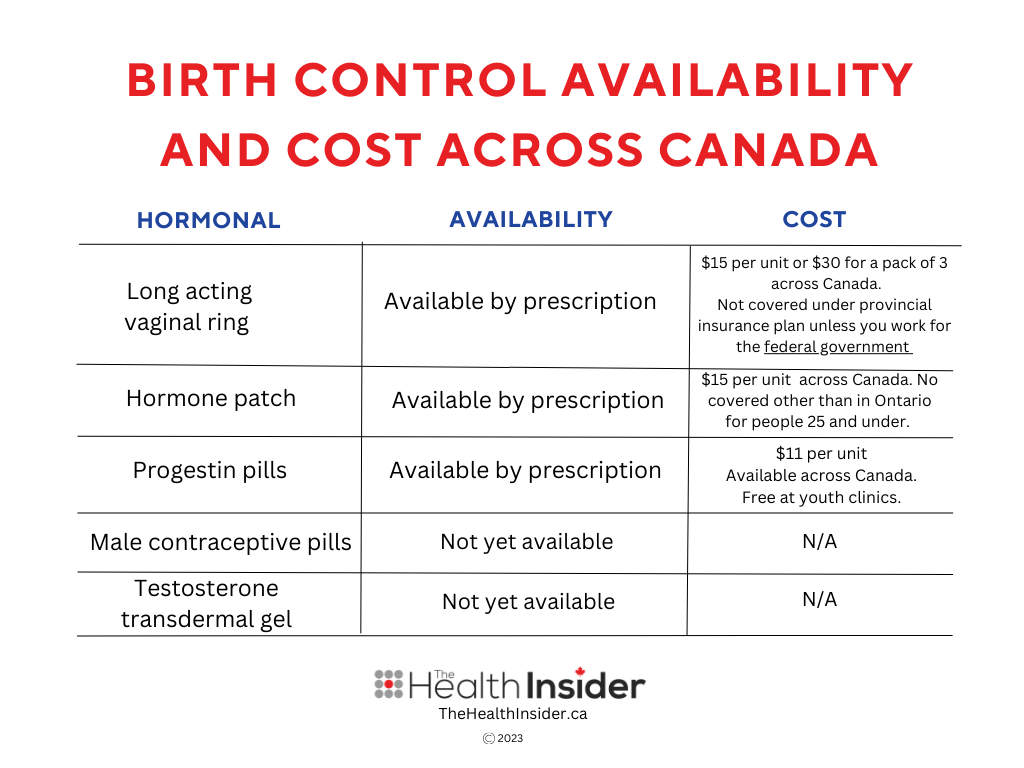
Cost and Coverage
British Columbia offers free contraception for many – but not all – birth control methods.
Ontario provides free birth control through OHIP+ and ODB for those under 25. None of the other provinces offer coverage for birth control, although there is a movement afoot to follow in B.C.’s footsteps.
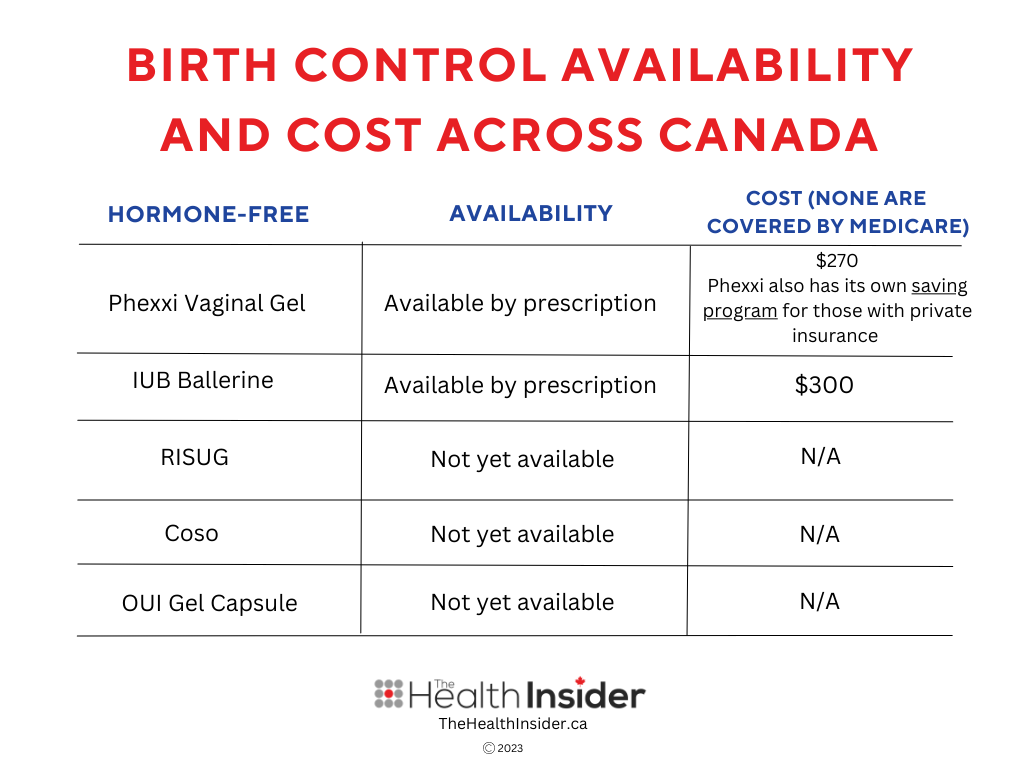
See below for a chart outlining the new hormonal options and their availability and cost in Canada. Stay tuned to The Health Insider for updates to this list.
Non-Hormonal Methods for Consideration
Non-hormonal options have gained popularity for their modern approach to birth control.
Unlike hormonal birth control, this approach is known to cause minimal side effects. Read on for some of the most promising options below.
- IUB Ballerine
This technique functions like a hormonal IUD, however it is much smaller in size and designed to cause less pain during insertion. IUB Ballerine works by releasing small amounts of copper, which functions as a spermicide. It can be used for up to five years and must be inserted by a healthcare professional.
The only significant side effects observed in trials were heavier and longer periods, however this resolved itself two to three months after insertion. With no impact on ovulation or mood, and an efficacy of 99 per cent, this technique appears to be comfortable and promising.
However, as with other IUDs, there is a risk of the IUD accidentally expelling itself from the body, which is seen in up to 11 per cent of cases. Additionally, the IUB can become malpositioned in the uterus. While rare, the occurrence was around 11 per cent in researched cases.
- OUI Gel Capsule
This gel works by inserting a tiny capsule into the vagina where it dissolves and produces a naturally thick mucus barrier, impenetrable by sperm. OUI is still a beta product being tested in labs, so side effects and risks have not been reported as of yet. The OUI gel capsule has been reported in lab tests to reach 99 per cent efficacy minutes after insertion, with effects lasting for up to five hours.
- RISUG
RISUG is an injectable form of male birth control which works similar to a vasectomy. However, instead of snipping the vas deferens, the injected serum contains a gel that sticks to the inner walls of the tubes and damages any passing sperm. This negatively impacts motility and effectively prevents the sperm from reaching the oocyte.
While RISUG remains in clinical and preclinical trials around the world, no adverse side effects have been recorded as yet, and it is said to have 99 per cent efficacy, lasting for up to 10 years.
- Coso
Coso is an intriguing and inventive ultrasound based male birth control option created by German inventor Rebecca Weiss. This is an at home device which halts sperm motility in the testicles.
Water is heated up in the Coso and the testes are placed in it. After stimulation with ultrasound waves for a few minutes, the Coso offers a short-term mode of birth control.
Efficacy ratings and side effects are unknown as the Coso is still undergoing trials.
- Phexxi
Phexxi is a vaginal gel which can be used at home. It can be inserted in the vagina no more than an hour before sex. This gel works by lowering the pH in the vagina, making it difficult for sperm to move towards the egg.
Phexxi reportedly has an efficacy of 93 per cent, however in reality this number is much lower at 86 per cent. It is said that this method works great with other birth control options such as condoms.
Common side effects include:
- Irritation to the vagina
- Yeast infections
- UTIs
- Bacterial vaginosis
Phexxi is generally safe to use while breastfeeding, or if one has recently given birth. However, it should not be used during pregnancy.
Changes to coverage and availability are made constantly as new information comes to light, so consider consulting a nearby pharmacy or your healthcare provider to confirm availability and coverage offered.
The Future of Birth Control
Notably, hormonal birth control is much more accessible than non-hormonal birth control. This can be attributed to the relative novelty of the latter option.
While the majority of hormone-free birth control options are still in the clinical and preclinical phase, this has not stopped the surge in interest among the general population.
Driven by the low incidence of side effects, relative comfort, and ability to cater to a larger demographic, the Health Insider team is eager to see safe and effective birth controloffered to Canadians.
Options for male birth control is a welcome change. Although limited, general awareness around the need for male birth control has paved the way for more research on the various birth control targets in the male reproductive system.
This is an exciting time for the field of pregnancy prevention. Even more exciting is the fact that male birth control tends to have fewer side effects than female birth control!
In the near future, we hope to see these efforts by the scientific community translated into more inclusive, accessible, safer, and healthier birth control options for all Canadians.
The information provided on TheHealthInsider.ca is for educational purposes only and does not substitute for professional medical advice. TheHealthInsider.ca advises consulting a medical professional or healthcare provider when seeking medical advice, diagnoses, or treatment.