Awareness of the pelvic floor and the all-important “Kegels” exercise was heightened in the early aughts when Sex and the City’s Samantha famously declared that she was “doing mine right now” while dining at a New York restaurant with her gal pals.
The fictional character Samantha knew what she was talking about. The pelvic floor is important not just for sexual function (Samantha’s main preoccupation), but also for overall health for both men and women.
What is the Pelvic Floor?
The pelvic floor is a formidable hammock of intricately connected muscles, ligaments and connective tissues that line the pelvis. It cradles the bladder, urethra, bowel, rectum, large intestine as well as the vagina and uterus in females and the prostate in males.
This indispensable network provides us with bladder and bowel control, support and stability for the spine, sexual function, and it works very, very hard during pregnancy and childbirth.
Women suffer from pelvic floor dysfunction more than men; upwards of 40% of women in Canada will experience pelvic organ prolapse and suffer from some form of pelvic floor dysfunction while 16% of men live with incontinence and 10% with pelvic pain.
Nearly 45% of those with symptoms never mention it to their doctor or health professional due to embarrassment, worry and stigma.
Causes of Pelvic Floor Dysfunction
Unsurprisingly, pregnancy and childbirth are one of the main causes of pelvic floor disorders among women.
Pregnancy and the resulting changes to the pelvic floor can cause postpartum pelvic floor dysfunction regardless of whether you give birth vaginally or by caesarian. Multiple births, instrumental births (e.g. use of forceps or vacuum), or perineal tearing increase the risk of pelvic floor damage.
Menopause is a time when many women notice various signs of pelvic floor dysfunction whether they gave birth or not. The condition at this time of life is known as the genitourinary syndrome of menopause (GSM). It occurs because the lack of estrogen causes thinning of the vagina (vaginal atrophy) and is believed to reduce the strength of the connective tissue supporting it.
Watch the informative video below from Alberta Health if you’re a woman seeking to learn in-depth about your pelvic floor health.
Both men and women are at risk if they suffered pelvic trauma or chronic constipation, sit for long durations, are obese, or regularly lift heavy objects. Additionally, urinary incontinence is very common after a prostatectomy.
Signs of Pelvic Floor Dysfunction
Both men and women may feel similar symptoms of pelvic floor dysfunction. These can include:
- Constipation and/or bowel straining.
- Ongoing pain in the pelvic area, genitals, or rectum.
- Leaking urine during exercise or while laughing, coughing, or sneezing (stress incontinence)
- Feelings of urgency to use the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficulty emptying the bladder.
- The feeling of needing to have several bowel movements over a short period of time.
- Pain in your lower back that cannot be explained by other causes.
Symptoms specific to women include:
- Pain or numbness during intercourse.
- Prolapse – may feel like a bulge in or coming out of your vagina, or a feeling of heaviness, discomfort, pulling, dragging or dropping sensation.
Symptoms specific to men include:
- Prolapse – may feel as though there is a bulge/ pressure in the rectum or an urgent feeling of needing to use your bowels.
- Pain in the testicles, penis or pelvis during intercourse.
- Erectile dysfunction.
- Painful ejaculation.
- Premature ejaculation.
Lifestyle Changes
Your treatment plan will depend on the cause of your dysfunction and the symptoms you are experiencing.
A variety of healthcare providers treat pelvic floor dysfunction. Depending on the cause and severity of your condition, a combination of experts may provide the best outcome for you.
The first stop for many will be their GP who may advise behavioural changes. These can include a Kegels exercise regime, heel slides, marches, diaphragmatic breathing and more.
Watch the video below for the top 5 pelvic floor exercises you can do at home.
Additionally, they may advise you to avoid pushing or straining when urinating or having a bowel movement and to learn how to relax the muscles in the pelvic floor area. Weight loss and smoking cessation may also help along with regulation of food and fluid intake such as caffeine-containing drinks.
Pelvic Floor Physiotherapy and Other Options
If lifestyle changes aren’t making a difference, you may want to up your game and see a pelvic floor physiotherapist.
Insider Tip: Pelvic Floor Physiotherapists are considered the first line of treatment for pelvic floor rehabilitation. They also help with preventive therapy which is particularly important for women considering pregnancy.
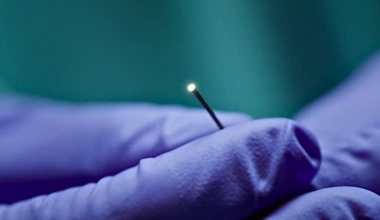
Physiotherapists may use a variety of treatments including biofeedback, pelvic floor electrical stimulation, magnetic therapy/neuromodulation, or weighted vaginal cones.
A popular new, non-invasive treatment is the EMSella chair, which is approved by Health Canada as a treatment for pelvic floor dysfunction. The chair promises to deliver 10,000 Kegels in a half hour, a compelling promise for many suffering from pelvic floor dysfunction. Other medical practitioners offer treatments such as laser therapy that stimulates collagen production and may provide relief of symptoms.
If exercise and working with a physiotherapist hasn’t helped with the condition, medical intervention may be the best option for both men and women. If you and your healthcare team agree, you may undergo surgery with your urologist or urogynecologist for stress incontinence or pelvic organ prolapse to finally help resolve the issue.
Unfortunately, surgical wait times are extremely long in Canada for any kind of gynecological surgery, and prolapse surgery is no exception. The average wait time in a public hospital in 2017 was 210 days, some of the longest wait times for any surgery across the country.
Cost
Pelvic floor physiotherapy is not covered under any provincial Medicare plan; however, it is covered by most private insurance plans. Some may ask for a doctor’s referral so check with your provider to see if this is the case.
Costs will range anywhere from $100 per session and up, depending on your needs.
Private gynecology and urology clinics are available around the country, however treatment they provide may not be covered by Medicare. The cost of private surgery for stress incontinence and organ prolapse can vary from clinic to clinic, so make sure you get all costs up front before proceeding.
Pelvic floor health is so important that since 1985, the French government officially subsidizes up to 20 sessions of physiotherapy to help tone the pelvic floor for all postpartum women. While we’re not quite as lucky here in Canada to have this kind of proactive postpartum pelvic floor care, there’s a lot you can do on your own to take charge.
Whether you’re male or female, you can turn to the plethora of skilled physios and medical professionals around the country who can help you on your journey towards long-lasting pelvic floor health.
It’s an excellent investment.
~ Read more from The Health Insider ~
- How to Find and Report Your Child’s Vaccine RecordsDon’t let lost paperwork lead to school suspension. Follow our “Record Rescue” checklist and learn about the CANImmunize app today.
- Why “Tech Neck” is a Growing Pain for CanadiansCanadians spend over 6 hours a day on devices. PT Sameer Chunara shares essential information to manage the 12kg of extra pressure on your cervical spine.
- The Shingles “Blind Spot”: Why 55% of At-Risk Canadians Are Unaware of Their Vulnerability55% of older Canadians with chronic diseases don’t know they are at higher risk for shingles. Learn about what you can do.
- Is Your Gut Contributing to Social Anxiety? New Science ExplainsDiscover the “microbiome-first” approach to social anxiety. Learn how bacteria, diet, and new therapy techniques are changing mental healthcare.
- Is an AI Redesign the Answer to Canada’s Healthcare Wait Times?Discover how a system-wide AI redesign could revolutionize Canadian healthcare productivity, diagnosis, and drug discovery according to the Fraser Institute.
- New CPR Guidelines for Canada: Why “Rescue Breaths” are Back for KidsHeart & Stroke’s updated guidelines emphasize that children need rescue breaths during CPR, as their cardiac arrests are typically oxygen-related.
The information provided on TheHealthInsider.ca is for educational purposes only and does not substitute for professional medical advice. TheHealthInsider.ca advises consulting a medical professional or healthcare provider when seeking medical advice, diagnoses, or treatment. To read about our editorial review process click here.